Abstract
Introduction: Multiple Myeloma (MM) is a rare hematologic malignancy, accounting for 12% of all hematologic cancers. Conventional treatment includes a combination of induction chemotherapy followed by stem-cell transplantation (SCT) for younger patients without significant renal impairment. While the efficacy of SCT in various clinical settings of MM are frequently explored, real-world data on impact of SCT on healthcare resource use (HRU) and costs among patients with MM are limited. This study compared HRU and costs for MM patients with and without SCT in the US.
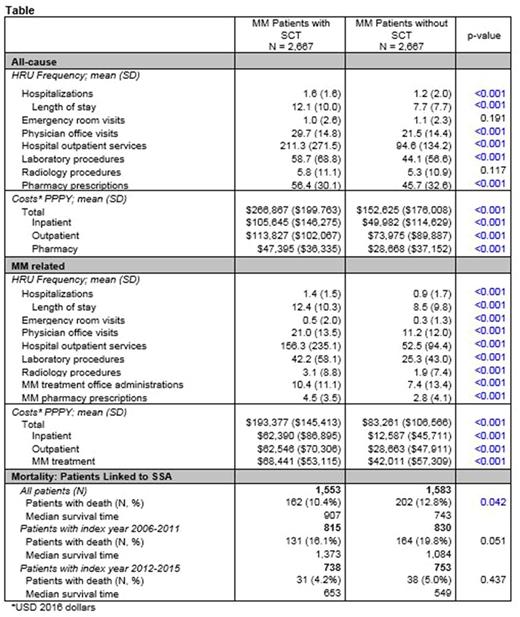
Methods: This retrospective analysis used the MarketScan administrative claims data to select patients newly diagnosed with MM (ICD-9-CM 203.0x) and at least 18 years of age during 7/1/2006- 9/30/2015 (first MM diagnosis = index date). Continuous health plan enrollment for 12 months prior to (baseline) and >3 months after index date (minimum follow-up) was required. Patients were censored at the earliest of disenrollment, death (inpatient or from the social security administration [SSA] death index), or end of study period (12/31/2015). Per-patient per year (PPPY) all-cause and MM-related HRU and costs were calculated during follow-up and compared between patients with SCT versus [vs.] without SCT. MM-related HRU and medical costs required a MM diagnosis code on the claim (primary discharge diagnosis for hospitalizations, any position on the claim for outpatient services). Costs were adjusted to 2016 USD using the medical component of consumer price index. Propensity scores were used to match patients 1:1 on baseline demographic and comorbid conditions using the nearest neighbor approach to adjust for differences between patients with and without SCT.
Results: Of the 14,229 newly diagnosed MM patients selected for analysis, 18.8% (N=2,669) received a SCT, of which 99.9% (N=2,667) were matched to MM patients without a SCT. Matched patients were well balanced on the following criteria: age (mean 56.7 [SD 8.2] and 57.4 [SD 8.5] years); gender (57.4% and 57.5% male); Charlson comorbidity index (mean 1.7 [SD 2.2] and 1.7 [SD 2.1]); baseline individual comorbid conditions (anemia [32.3% and 30.9%], renal impairment [7.0% and 6.5%], bone-related [32.6% and 30.3%], cardiac dysfunction [36.4% and 36.0%]). Total all-cause and MM-related healthcare costs PPPY were $114,242 and $110,116 higher among patients with a SCT (vs. patients without a SCT). Similarly, patients with a SCT (vs. patients without a SCT) incurred $55,663 and $49,803 higher all-cause and MM-related costs for hospitalizations, and $39,852 and $33,883 higher all-cause and MM-related costs for outpatient services. MM treatment costs (drug and administration costs) PPPY were also $26,430 higher among patients with a SCT (vs. patients without a SCT). Higher costs among patients with a SCT were driven by increased HRU for both inpatient and outpatient services across the majority of categories (Table). Among the subset linked to the SSA death index (SCT N= 1,553 and non-SCT N=1,583) the median survival time 907 vs 743 days (p<0.001) among patients with a SCT vs. patients without a SCT and the proportion with a death was 10.4% and 12.8% (p=0.042). The difference in median survival time between groups was less pronounced for patients with an index date in a later year; 2006-2011 vs. 2012-2015 (Table).
Conclusions: Results show that among age-, gender-, and comorbidity- matched MM patients, management with SCT is associated with higher all-cause and MM-related HRU and costs and increased survival. An examination of the predictors of management with or without SCT and associated outcomes will inform the relative value of therapeutic strategies for MM patients as well as help optimally triage healthcare resources.
Ailawadhi: Pharmacyclics: Research Funding; Novartis: Consultancy, Honoraria; Amgen: Consultancy, Honoraria; Takeda: Consultancy, Honoraria. Panjabi: Amgen Inc.: Employment, Equity Ownership. Princic: Truven Health Analytics, IBM Company: Employment. Fowler: Truven Health Analytics, IBM Company: Employment. Tran: Truven Health Analytics, IBM Company: Employment. Gatta: Amgen Inc.: Employment, Equity Ownership. Medhekar: Amgen Inc.: Employment, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.